The CY 2024 Home Health Final Payment Rule introduces a wave of changes, including updates on the comorbidity adjustments.
The final rule reads: “only those subgroups of diagnoses that represent more than 0.1 percent of periods of care and that have at least as high as the median resource use will receive a low comorbidity adjustment. This is based on the knowledge that the average number of comorbidities in the aggregate becomes the standard within that population for the purpose of payment. However, because we still expect HHAs to report all secondary diagnoses that affect care planning, there will be comorbidity subgroups included in the home health-specific list that do not meet the criteria to receive an adjustment.”
Low Comorbidity Adjustment Subgroups
In 2024, there will still be 22 Low Comorbidity Adjustment Subgroups, but significant changes are underway. Specifically, the following diagnoses will be removed from the low comorbidity adjustment subgroup. This implies that if any of these diagnoses are now listed as comorbidities in slots 2-25, you will no longer be eligible for a low comorbidity adjustment.
- Gastrointestinal 1 – Crohn’s, Ulcerative Colitis, and other Functional Intestinal Disorders
- Musculoskeletal 2 – Rheumatoid Arthritis
- Neoplasm 6 – Malignant neoplasms of the trachea, bronchus, lung, and mediastinum
Conversely, the following will be added to the low comorbidity adjustment subgroups:
- Neoplasms 17 – Secondary neoplasms of respiratory and GI systems
- Neurological 4 – Alzheimer’s disease and related dementias (including G30.9 Alzheimer’s disease, unspecified)
- Respiratory 10 – 2019 Novel Coronavirus (U07.1 COVID-19)
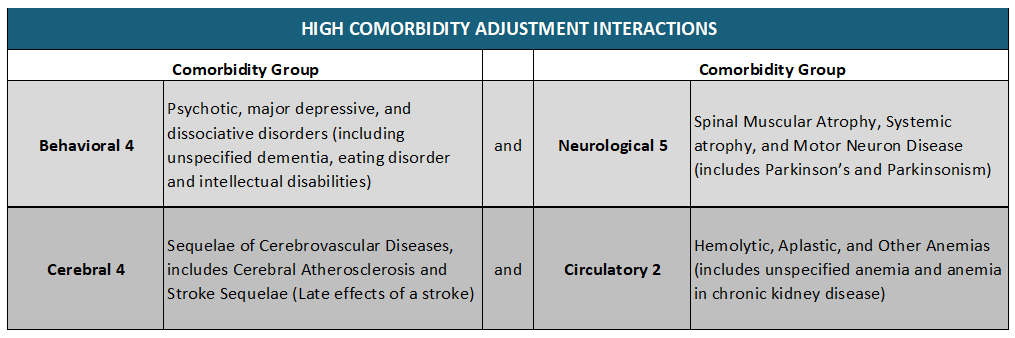
High Comorbidity Adjustment Interactions
For High Comorbidity Adjustment, 11 additional comorbidity group interactions will be added increasing the number from 91 (in 2023) to 102. Below are some examples of the newly added comorbidity group interactions.
A combination of these codes in positions 2-25 on the claim will result in a positive adjustment to the reimbursement value.
Comorbidity adjustments have a significant impact on your reimbursements, so make sure your coders are well aware of these changes and properly apply them accordingly as they assign codes.

