[UPDATED] On March 26, CMS announced the extension of the phased-in participation of the Review Choice Demonstration for Home Health Agencies in Florida and North Carolina for an additional 90 days starting April 1st.
Between April 1 and April 15, providers who participated in Cycle 1 were given the chance to choose from a subsequent choice selection for Cycle 2 which will begin on May 1st.
If your agency has chosen the Pre-Claim Review, here are some factors that can lead to non-affirmation:
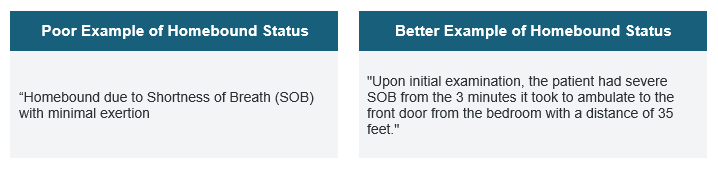
Homebound Status
As a basic requirement for eligibility, all home health claims should meet Medicare’s criteria 1 and 2 for a patient’s homebound status. Most non-affirmed claims related to the homebound status fall under any of these three specific reasons:
- The submitted documentation does not support homebound criteria; only one is met.
- The submitted documentation does not support a normal inability to leave home.
- The submitted documentation does not support a considerable and taxing effort to leave home.
Qualities that Negate Homebound Status
- No coordination or balance problems
- No need for assistive devices
- Have the ability to walk independently on even surfaces
- Independent with transportation
- Frequently goes out of the home for a non-medical reason
Face-to-face Encounter
Oftentimes, non-affirmed claims related to a face-to-face encounter have an invalid physician certification due to the following reasons:
- The required face-to-face encounter document is missing.
- The required face-to-face encounter is untimely and/or the certifying physician did not document the date of the encounter.
- The required face-to-face encounter is not related to the primary reason for home health services.
The certifying physician must include in the documentation of the encounter a note describing how the patient’s clinical condition during that encounter supports the patient’s homebound status and need for skilled services. The face-to-face encounter must occur no more than 90 days prior to the home health start of care date or within 30 days after the start of care. The certifying physician must document the encounter either on the certification, which the physician signs and dates, or on a signed addendum to the certification.
Therapy Services
Ensure that the submitted documentation supports the medical necessity of the therapy services. Medicare is critical in reviewing the therapy and other skilled services. Most often, the reasons for non-affirmation are as follows:
- Documentation submitted does not include measurable physical therapy treatment goals that are related to the patient’s illness, injury, or impairment.
- Documentation submitted does not support that physical therapy services are reasonable and necessary and at a level of complexity that requires the skills of a qualified therapist.
- Documentation submitted does not include specific therapy goals.
- An order for therapy services is invalid because it does not contain either the type and frequency of services to be provided or the professional who will provide the services.
Preparing your agency for RCD
Many lessons can be pulled from the abovementioned reasons for non-affirmation, which can guide an agency in establishing new documentation protocols. Two things are key to succeed in Pre-Claim Review and RCD in general: (1) timeliness in submitting fully-compliant medical documentation, and (2) close collaboration with providers to ensure availability of the documentation.
Illinois’ experience as the first state to undergo RCD proved that a significant amount of time and resources are needed for the additional tasks involved in ensuring that all required medical documentation is accurate and submitted properly.
Working closely with the Medicare Administrative Contractor (MAC) is important to fully understand the new administrative requirements that will impact an agency’s workflow and resources. This will also help give operational foresight even for agencies that are not in the current RCD states.
Resources:
CMS Updates: Review Choice Demonstration for Home Health Services >>
CMS: RCD for Home Health Services Operational Guide >>
CMS: RCD for Home Health Services FAQs >>
Palmetto: Pre-Claim Review Non-Affirmations: Homebound >>
Palmetto: Pre-Claim Review Non-Affirmations: Face-to-Face Encounter >>
Palmetto: Pre-Claim Review Non-Affirmations: Therapy >>

