Claims containing primary diagnoses that do not fall into one of the 12 PDGM clinical groups may be denied by CMS or sent back to the agency with a “Return to Provider” (RTP) remark. Such primary diagnoses are referred to as “Questionable Encounters” (QEs).
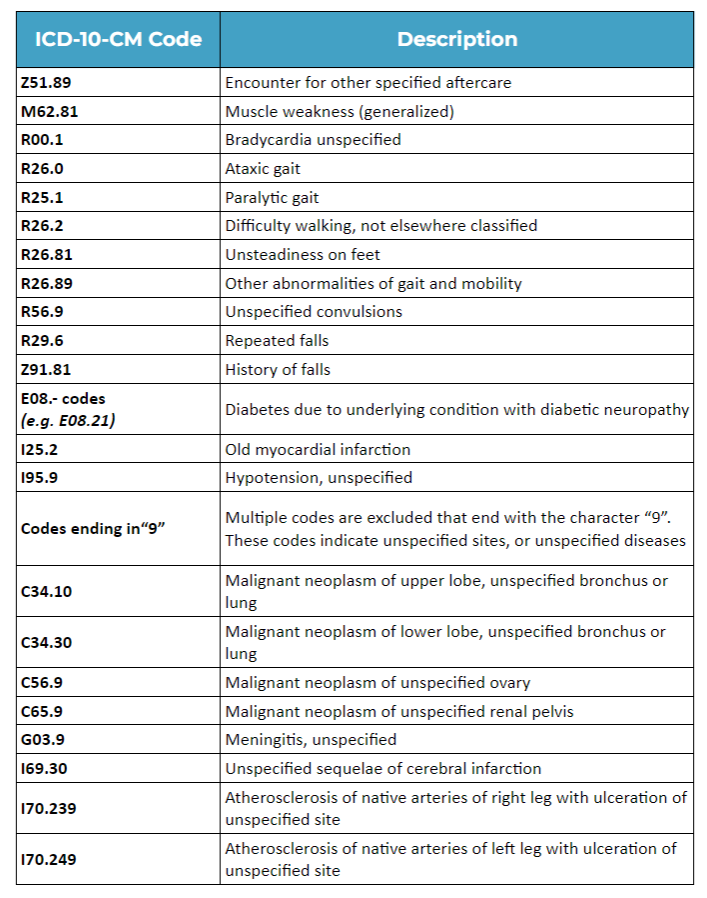
QE codes, like symptom codes, are often deemed “too vague” as they lack sufficient information to justify the need for home health services. Additionally, some diagnosis codes are simply not suitable for the home health setting. For example, muscle weakness, which can result from various causes, prompts CMS to search for the underlying cause for accurate assessment. Below are top 25 QE codes from a previous data from CMS:
Top 25 QE Codes
5 Tips to Avoid QEs:
- Provide ongoing re-education for intake, quality assurance, and coding teams on checking and recognizing diagnosis codes that will not be associated with a clinical grouping under PDGM.
- Clearly communicate with your referral sources about the importance of precise documentation and diagnosis coding to substantiate home health services and avoid return-to-provider claims.
- Implement measures to ensure accurate and substantive clinical documentation practices internally, that support patient complexity, homebound status, and skilled need. CMS expects clinicians to investigate the cause of symptom codes, obtain provider confirmation, and assign the appropriate code accordingly.
- Review your current coding trends and previous claims, particularly those with primary diagnoses that may be considered questionable encounters under PDGM. Educate your staff on appropriate coding with emphasis on the focus of care. This should involve educating your clinical team to ensure that their treatment plans are centered on addressing the underlying cause of the disease or impairment, rather than focusing solely on symptoms.
- Avoid using unspecified codes, coding etiology before manifestation, symptom codes as the primary code, inappropriate acute conditions, and diagnosis codes that do not support the need for home health.
For instance, if a patient has muscle weakness due to COPD-related inactivity, code for COPD. Document muscle weakness using manual muscle testing scores, functional assessment findings, and clinical observations. Similarly, code for lower extremity osteoarthritis instead of “gait abnormality” to accurately reflect the medical condition causing the abnormal gait.
Gain further insights into identifying the appropriate code to use instead of questionable encounter codes in this resource from Axxess Home Health>
For more information and a comprehensive list of questionable encounters in home health, you may refer to this resource from the National Association of Home Care and Hospice>

